Cervical Spine
This illustration is reproduced with permission from the Surgery of the Cervical Spine pamphlet (RACS, NSA, Mi-tec Medical Publishing). The complete pamphlet is available from your surgeon.
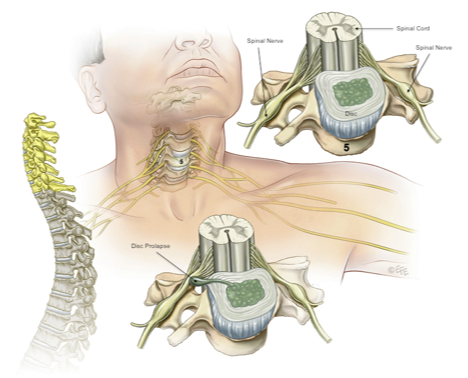
The cervical spine is made up of 7 vertebrae from the base of the skull to the top of the chest. Each vertebral body has a disc above and below. Behind the vertebrae and discs is the spinal cord, surrounded by CSF (cerebrospinal fluid) and the meninges (membranes). At each disc level, a nerve leaves the spine on each side, and runs into the upper limb to supply the muscles and skin of the arms and hands. The vertebrae are numbered from C1 to C7. The nerve roots are numbered from C1 to C8 (C1 nerve leaves above the C1 vertebra; C8 nerve leaves below the C7 vertebra). The discs are numbered according to the adjacent vertebral bodies, so the disc between vertebra C6 and C7 is referred to as the C6-7 disc, and the C7 nerve root leaves the spine at this level.

In this MRI picture, the cervical vertebrae and the intervening discs (short white arrow) are seen, with the spinal cord (long white arrow) surrounded by CSF (double white arrow).
Each cervical disc is made up of a tough fibrous membrane (annulus fibrosis) that surrounds the soft centre (nucleus pulposus). If there is a tear in the annulus, the nucleus can herniate (prolapse) through the annulus and compress the spinal cord or the nerve root. If the disc compresses the nerve root, then the nerve causes pain in the arm or hand, and may produce numbness and weakness. This is called cervical radiculopathy. If the disc prolapse compresses the spinal cord, then the spinal cord may be injured, and result in a form of quadraparesis or quadraplegia. This is called cervical myelopathy. This causes weakness and numbness in the arms and legs, in addition to problems with bladder and bowel function.
The diagnosis is made by performing an MRI of the cervical spine. Other tests that may be required are flexion/extension Xrays of the neck, and cervical CT myelography.
The treatment of cervical disc prolapse depends on:
The diagnosis is made by performing an MRI of the cervical spine. Other tests that may be required are flexion/extension Xrays of the neck, and cervical CT myelography.
The treatment of cervical disc prolapse depends on:
- The presence of myelopathy or radiculopathy
- The duration of symptoms
- The age of the patient
- Associated medical problems
- The severity of the disease
For those with a disc prolapse and neck pain, but no radiculopathy or myelopathy, then surgery is not required, and treatment is managed by the general practitioner and physiotherapist. There should never be chiropractic treatment on the cervical spine.
For those with radiculopathy, treatment by the general practitioner and physiotherapist is used for 6-8 weeks. With appropriate pain relief (analgesic medication), strict attention to posture, and a regular walking programme, most patients’ symptoms settle during this time. If symptoms fail to settle during this time, or symptoms become worse, then surgery is required.
In all patients with cervical myelopathy, surgery is required to prevent progression to total quadraplegia.
There are many different types of surgery used in the cervical spine. The type of surgery used in each case depends on the extent of injury seen on the MRI, the posture of the cervical spine, the patient’s age, and the surgeon’s experience/preference. The operations are generally divided into 2 groups, (i) anterior (from the front), and (ii) posterior (from the back).
For those with radiculopathy, treatment by the general practitioner and physiotherapist is used for 6-8 weeks. With appropriate pain relief (analgesic medication), strict attention to posture, and a regular walking programme, most patients’ symptoms settle during this time. If symptoms fail to settle during this time, or symptoms become worse, then surgery is required.
In all patients with cervical myelopathy, surgery is required to prevent progression to total quadraplegia.
There are many different types of surgery used in the cervical spine. The type of surgery used in each case depends on the extent of injury seen on the MRI, the posture of the cervical spine, the patient’s age, and the surgeon’s experience/preference. The operations are generally divided into 2 groups, (i) anterior (from the front), and (ii) posterior (from the back).
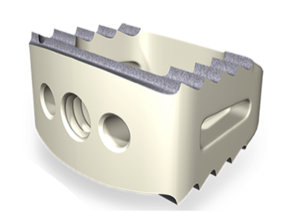
Some surgeons have tried using a different spacer, called a disc arthroplasty or disc replacement. Careful analysis of disc arthroplasty has not demonstrated any benefit compared with ACDF with a cage.
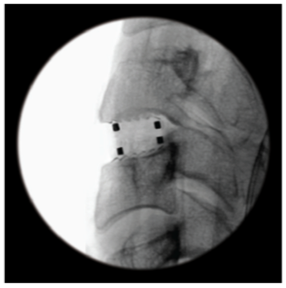
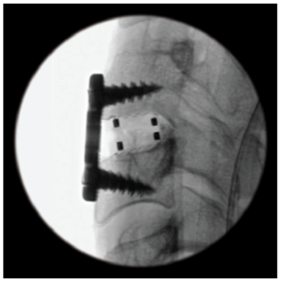
XRays demonstrating a single cervical cage (left) and a cage with a cervical plate (right).


XRays demonstrating postoperative result with C6-7 ACDF
Posterior surgery involves removing part of the back of the spine (lamina), but leaving the disc alone. Foramenotomy involves removing a tiny part of the lamina and the adjacent joint (called the facet joint) to decompress the nerve root. A laminectomy involves removing the whole lamina, to take pressure off the spinal cord. Sometimes, insertion of screws and rods into the spine is required after a laminectomy.